In Clinical
Follow this topic
Bookmark
Record learning outcomes
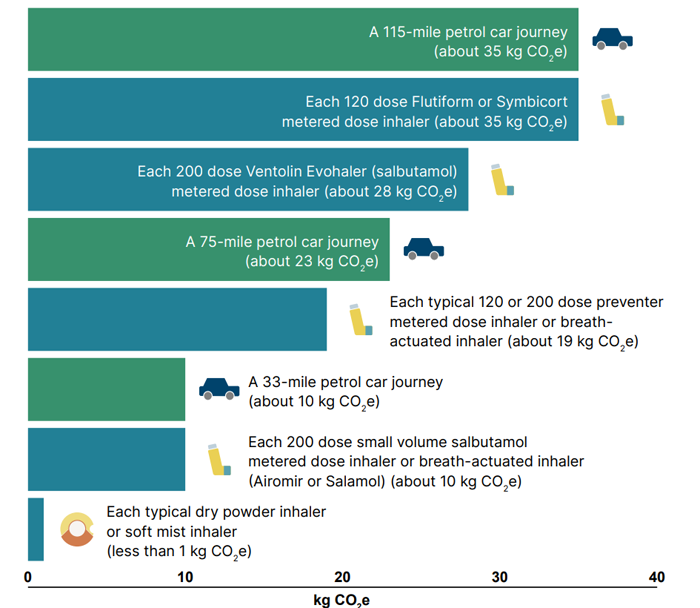
Pressurised metered dose inhalers (pMDIs) use hydrofluoroalkanes (HFA) as propellants — powerful greenhouse gases up to 3,000 times more potent than carbon dioxide. In the UK, pMDIs account for 70 per cent of inhalers prescribed (higher than many other European countries). Short- acting beta-agonists (SABA) are usually prescribed as pMDIs, with salbutamol accounting for most of the carbon footprint associated with inhalers.
To help with decision-making, Greener Practice (greenerpractice.co.uk) has published a guide which breaks down the carbon footprint of each inhaler, as does Bulletin 295 published by PrescQuipp, while MIMS now contains a table listing carbon emissions from inhalers.
Additionally, NICE, the Scottish Intercollegiate Guidelines Network (SIGN) and the British Thoracic Society (BTS) have produced a patient guide to support informed decision-making, again listing the impact of each inhaler and specifically calling out the most detrimental to the environment (Ventolin Evohaler, Flutiform and Symbicort, when compared to other inhalers with the same or similar active ingredient[s]).
Role of pharmacy teams
Seventy-five per cent of the population are concerned about climate change and adults reporting concern were three times more likely to make lifestyle changes to make a difference. Patients with lung conditions are most impacted by environmental factors; their appreciation of this positions them well for wanting positive change.
Pharmacy teams are ideally placed to make a difference with opportunities for patient intervention and counselling when handing in/collecting prescriptions or during a NMS review. Collaborating with GP practices and asthma clinics will help reinforce patient messages.
At the point of diagnosis and during any subsequent reviews, the Assess, Choose, Train decision tool is helpful (see Figure 1). This ensures the patient is part of the decision, an appropriate inhaler type is chosen and the patient is able to use it effectively – which helps aid adherence, improve condition control, reduce the need for rescue medicines and ultimately hospital admissions, thereby avoiding the carbon footprint impact of poor control.
Optimising condition control
Review inhaler prescription history – identify asthma patients who have had three or more short-acting bronchodilator inhalers in the last six months with no inhaled corticosteroid prescription, explain impact on control and refer them for an asthma review*
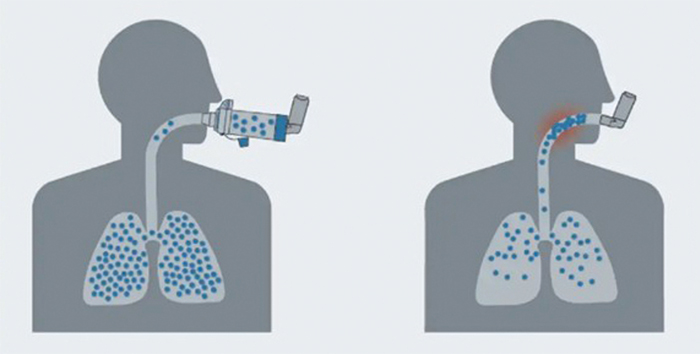
Identify children aged between five and 15 years using pMDIs and check they have a spacer device and know how to use it properly. Refer to GP/clinic if they don’t have a spacer.*
When counselling patients with SABA prescriptions, identify those using the inhalers >3 times a week
Recommend a spacer device to all patients as needed, if not already using one
Contact local surgeries to understand their protocols for prescribing, reviewing frequency of prescriptions, spacer advice, inhaler technique training and referral pathways
Are your patients equipped to self-manage exacerbations? Do they have an emergency treatment pack?
Inhaler choice
Familiarise yourself with the NICE patient decision aid and use this when counselling
Encourage patients to consider whether they would be a candidate for switching to a DPI (able to breathe in quickly and deeply through the mouth within two to three seconds)
Reassure patients that they can switch back if there is any negative impact on condition control
Signpost patients to new information published in conjunction with NHS England on the Asthma + Lung UK website.
Use the Assess, Choose, Train decision tool techniques (see Figure 1) to help patients understand if they are able to use a DPI
Use an In-Check DIAL to coach DPI or pMDI inhaler technique
Describe the impact of inhalers using local distances travelled in a car (see Figure 3).
Minimise impact (if pMDIs are clinically needed)
Identify any inhaler users where prescribing can be rationalised (e.g. from two puffs of 100mcg to one puff of 200mcg).
Understand the different carbon footprints of each pMDI and discuss with your surgery if there is a way to minimise their impact through local prescribing protocols.
Improve technique and adherence
Complete CPPE inhaler technique training and assessment*
Check inhaler technique as part of the NMS and include patients switching to a new device*
Counsel all patients on the importance of good inhaler technique
Check that all patients aged five years and above with an inhaler for asthma have a personalised asthma action plan (PAAP). Refer appropriately if no PAAP.*
Signpost to patient videos on Asthma + Lung UK website
Ask patients about their PAAP/COPD management plan – are there any areas that you can support?
Identify patients for an inhaler technique check every three months
Identify patients on multiple types of inhalers (e.g. DPI, pMDI and SMI), discuss techniques and refer for rationalisation as appropriate.
Patient returns
Train everyone on inhaler waste management*
Ask patients presenting with inhaler scripts: “Do you have any inhalers to return today?”*
On hand-out, counsel patients to return all unwanted and used inhalers for safe disposal referencing environmental impact.*
Explore whether there are any local inhaler recycling schemes in your area
Encourage local GP surgeries to counsel on safe returns and the impact of this on the environment to reinforce your communications
Add information to dispensing labels to encourage inhaler returns to your pharmacy.
Summary
While the environmental impact of inhalers needs to be reduced, this must be carried out without causing harm to patients. Control of symptoms is first and foremost, and any changes must involve the patient having enough information to make an informed choice regarding the carbon impact of different inhalers.
Recognise that patients may want to switch inhalers to minimise environmental impact and reassure them that they can switch back if their control is negatively impacted in any way. Three key actions that will make a difference are:
- Improving condition control and therefore reducing excess use of SABA inhalers
- Switching pMDIs to DPIs or SMIs if clinically appropriate
- Encouraging the correct and safe disposal of used inhalers through pharmacy returns.
As Pritchard and Usmani wrote in The Greenest Inhaler: A Patient-centric Approach: “The greenest inhaler is the one that a patient can and will use effectively and the greenest patient is the one whose respiratory condition is well controlled.”
*References are available from the Editor.

